Cardiooncology Munich
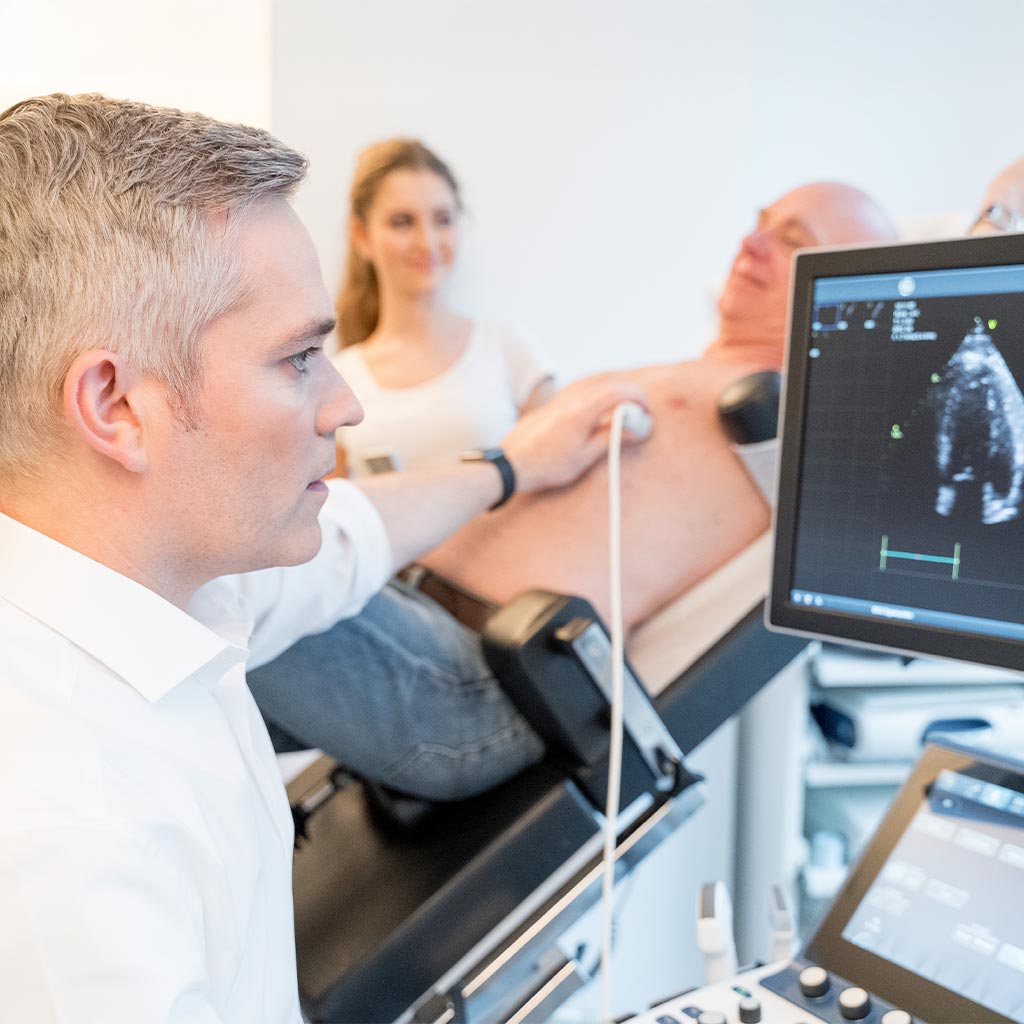
Taking good care of the heart before, during and after cancer treatment
For many people, cancer is a major physical and emotional challenge. In addition to the tumour itself, the necessary therapies can also put a heavy strain on the heart and circulation. To ensure that the treatment runs as smoothly as possible, oncology and cardiology need to work together. This is exactly what cardio-oncology offers: it helps to protect the heart during and after cancer therapy, to recognise risks in good time and to tailor treatment to individual needs.
In our specialist practice for cardiology in Munich we combine many years of experience with a high degree of empathy. We accompany you competently, personally and with a great deal of empathy through this sensitive time.